Blogs

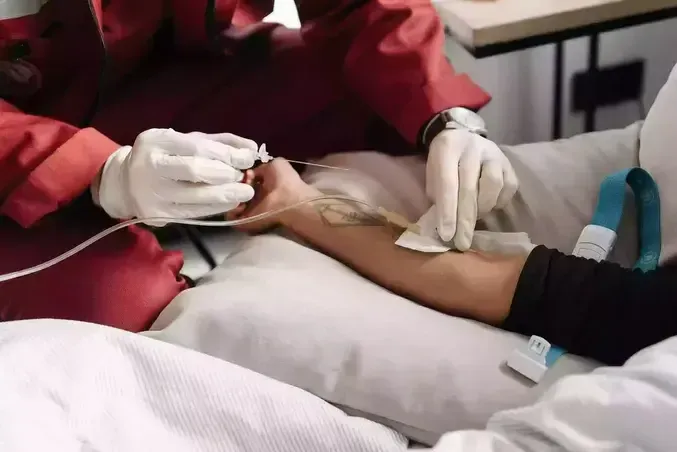
Research-Backed Telehealth Plus Rapid Response for Medically Complex Veterans in Family-Style Homes The One Critical Element That Makes It Work in Real-World Care Medically complex Veterans who live in small, family-style homes often do better with routine, relationship-based support, but they can also face higher risk for avoidable emergency room visits and hospitalizations when early warning signs are missed or when help cannot mobilize quickly enough. The most practical, research-backed solution is not simply “more monitoring.” It is pairing home telehealth with a rapid response capability that can act on what the data is signaling, before a manageable issue becomes a crisis. VA Medical Foster Home care in Cheyenne. When you combine continuous monitoring with timely clinical intervention, you create a safer care environment that supports stability, reduces stress, and strengthens continuity of care in the home. Evidence Base: Telehealth Plus Rapid Response Reduces ER Visits and Hospitalizations Below is the core intervention and implementation elements exactly as outlined: 1 Research-Backed Intervention to Reduce Avoidable Emergency Room Visits and Hospitalizations for Medically Complex Veterans in Small, Family-Style Homes—and the 1 Critical Element That Makes It Work Medically complex veterans living in small, family-style homes face higher risks of avoidable emergency room visits and hospitalizations. A research-backed intervention combining home telehealth with rapid response teams has shown measurable success in addressing this challenge. This article examines the evidence behind this approach and shares insights from healthcare experts who have implemented it in practice. Home Telehealth With Rapid Response Reduces Hospitalizations For example, the study demonstrated that remote monitoring programs significantly reduce emergency hospitalizations and emergency department visits among veterans with chronic conditions. The key elements for successful implementation in real-world practice are: Reliable technology — wearable devices, alert buttons, and sensors that track critical health indicators and automatically transmit data to the healthcare team. Rapid response — prompt assessment of alerts and timely intervention, such as physician consultation, therapy adjustment, or home visits. Integration with clinical workflows — data is accessible to the treating physician and used for personalized care. Family and caregiver support — training and involvement of close relatives enhances the effectiveness of the intervention and reduces patient stress. Karmela Rafael , Senior Care Specialist, Be Well Medical Alert The Critical Element That Makes This Intervention Work In practice, the critical element is rapid response. Monitoring alone does not prevent hospitalizations. Prevention happens when an alert triggers a clinically appropriate action fast enough to change the outcome. In a small, family-style home, this matters even more because: Changes can be subtle at first, especially with chronic disease, frailty, or complex medication regimens. A delay of hours can turn dehydration, a UTI, COPD flare, or medication side effects into an ED visit. Caregivers need a clear escalation pathway that does not rely on guesswork or waiting until symptoms are severe. If you want measurable reductions in avoidable utilization, rapid response is the operational bridge between “data” and “care.” What “Rapid Response” Looks Like in a Family-Style Home A strong rapid response model typically includes: Reliable technology: wearable devices, alert buttons, and sensors that track critical health indicators and automatically transmit data to the healthcare team. Rapid response: prompt assessment of alerts and timely intervention, such as physician consultation, therapy adjustment, or home visits. Integration with clinical workflows: data is accessible to the treating physician and used for personalized care. Family and caregiver support: training and involvement of close relatives enhances the effectiveness of the intervention and reduces patient stress. Implementation Checklist: How You Set This Up to Reduce Avoidable ER Visits If you are implementing this approach, focus on these operational essentials: Technology that is dependable and simple Choose devices that are easy to use, require minimal troubleshooting, and transmit reliably. Complexity increases failure rates, especially when multiple caregivers rotate. Response times that match medical risk High-risk patients need faster triage. If your model cannot respond quickly to meaningful alerts, you will not capture the full benefit. Workflow integration that supports real clinical decisions Data must be visible and actionable for the treating clinicians, not stored in a separate system that no one checks. Caregiver training that is repeated and practical Training is not a one-time event. It should include scenarios, escalation scripts, and reinforcement so the home responds consistently under stress. Why This Approach Fits Medically Complex Veterans in Small Homes Small, family-style settings can deliver exceptional stability when they are supported by the right clinical infrastructure. Telehealth monitoring strengthens early detection, and rapid response converts early detection into early intervention. That combination is what reduces avoidable emergency visits and hospitalizations while keeping the Veteran supported, safe, and cared for in the home environment. If you want, share your typical Veteran acuity profile (diagnoses, fall risk, oxygen use, polypharmacy, dementia, CHF, COPD, diabetes), and you will get a copy-paste-ready rapid response protocol outline with escalation thresholds that fits a small, family-style home model.